Context. The perhaps only CMML-specific Randomized Clinical Trial (RCT) established hydroxyurea (HY) as the main treatment (Tx) for advanced proliferative CMML (Wattel Blood 1996). In Europe, the only hypomethylating agent (HMA) approved in CMML is AZA in non proliferative CMML-2. Phase 2 trials reported the activity of decitabine (DAC) in advanced proliferative CMML (Braun Blood 2011, Santini Leukemia 2018). We performed a RCT of DAC (±HY during the first 3 cycles) vs HY alone in those pts.
Methods. The DACOTA trial (EudraCT 2014-000200-10) accrued pts with previously untreated (or < 6 weeks of HY), proliferative (WBC ≥ 13x109/L) CMML with advanced disease defined per Wattel et al as presence of extramedullary disease or ≥2 criteria among: BM blasts ≥5%, abnormal karyotype (except -Y), ANC ≥ 16x109/L, Hb < 10 g/dL, platelets < 100 x109/L or splenomegaly > 5 cm below costal margin. Pts were randomized 1:1 to DAC (20 mg/m2/d IV 5d/28d) or HY (1g/d, adjusted on WBC, 28d cycles) and treated until death, AML transformation or progression. The primary endpoint was EFS, events being death, transformation to AML, progression of myeloproliferation after 3+ cycles or progression of blasts and cytopenias after 6+ cycles. Response was assessed with IWG 2006 criteria modified to account for improvement of myeloproliferation, after central morphology review. Intent-to-treat analyses were done considering missing responses as failures.
Results. From Oct 2014 to Sep 2019, 217 pts from 47 centers were screened and 170 randomized (84 DAC and 86 HY), including 12 pts (6 DAC and 6 HY) who never started Tx. Median age was 73 years (IQR 68-78). WHO was CMML-NA/1/2 in 2, 114 and 54 pts, respectively (resp). Median WBC 34.9 x109/L (IQR 22.9-55.7). Cytogenetic risk (Such Haematologica 2011) was fav 69%, int 12%, adv 18% NA 1%. Mutations in TET2, SRSF2, ASXL1 and signaling genes (CBL, JAK2, FLT3, KIT, NRAS, KRAS and CSF3R) were present in 64%, 51%, 62% and 57% resp. 72 pts had received HY for a median 27 days prior to randomization.
Aside from older age in the HY arm (median 74 vs 71.5y in the DAC arm), there was no imbalance between Tx arms. DAC and HY pts received a median of 5 (IQR 3-12) and 6 (IQR 3-14) cycles, resp. As of 15th June 2020, 5 and 10 DAC and HY pts were still on Tx. Reasons for Tx cessation in the DAC arm were death (n=19), AML transformation (n=16), progression (n=9) , hematological toxicity (n=13) or other (n=21). Reasons for Tx cessation in the HY arm were death (n=14), AML transformation (n=13), progression (n=18), hematological toxicity (n=6) or other (n=20). 126 and 85 pts received 3 and 6 cycles, resp. In the ITT population, ORR at 3 cycles was 56% (7CR, 25 mCR±HI, 15 SD+HI) and 30% (0 CR, 8 mCR±HI, 18 SD+HI) in the DAC and HY arms, resp (p=0.0011) and ORR at 6 cycles was 32% (6 CR, 9 mCR±HI, 12 SD+HI) and 17% (2 CR, 4 mCR±HI, 9 SD+HI) in the DAC and HY arms, resp (p=0.033). Median response duration was 15.9 vs 18.2 months (mos) in the DAC and HY arm, resp (p=0.81). Infection and hemorrhage occurred at least once in 49% and 31% of pts, resp. 55% of DAC pts and 38% of HY pts required hospitalization at least once (p=0.05). Non-heme ≥ grade 2 AEs occurred in 79% and 63% of DAC and HY arms, resp (p=0.03). Grade ≥3 cardiac AEs occurred in 13 DAC and 4 HY pts, resp.
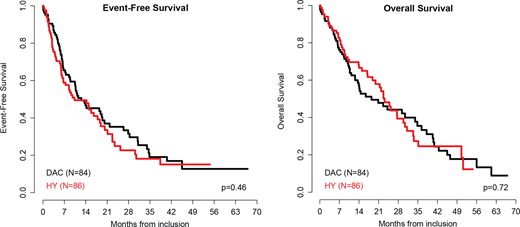
With a median follow-up of 13.9 mos, median EFS was 12.6 vs 10.3 mos in the DAC and HY arms, resp (reference DAC arm, HR= 1.14 CI95 0.8-1.64, p= 0.46). Median AML-free survival (AMLFS) was 13.6 and 15.8 mos in the DAC and HY arms resp (p=0.86). Median OS was 18.4 and 23.1 mos in the DAC and HY arms, resp (p=0.72). Considering death and AML transformation as competing risks there was no significant difference in cumulative incidence of AML (p=0.1) or death without transformation (p=0.06) between arms. 30 pts from the HY arm received an HMA (DAC n= 13, AZA n= 16, both=1) after study exit. Censoring at HMA onset in the HY arm, median OS was 18.4 vs 30.4 in the DAC and HY arm, resp (p=0.15). 13 pts were transplanted (DAC n= 10, HY n= 3). There was no interaction between Tx arm and CMML-0/1 vs -2, platelets ≥ vs <100 x109/L and anemia (Hb < 8 g/dL or RBC-TD vs Hb ≥8) on both EFS and OS (all p>0.05).
Conclusion. RCTs are feasible in advanced proliferative CMML, which remains an unmet medical need. In these pts, DAC did not provide an overall or event-free survival advantage over HY. HY remains a valid option in advanced proliferative CMML. However, one third of HY pts subsequently received an HMA and more DAC pts achieved a response and were bridged to HSCT.
Itzykson:Abbvie: Honoraria; Daiichi Sankyo: Honoraria; Otsuka Pharma: Membership on an entity's Board of Directors or advisory committees; Astellas: Honoraria; Sanofi: Honoraria; BMS (Celgene): Honoraria; Janssen: Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Stemline: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees; Oncoethix (now Merck): Research Funding; Karyopharm: Membership on an entity's Board of Directors or advisory committees. Santini:BMS, J&J, Novartis: Honoraria; Acceleron, BMS, Menarini, Novartis: Consultancy; Takeda, Pfizer: Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding. Lionel:Abbvie: Consultancy; Takeda: Consultancy; Celgene/BMS: Consultancy, Research Funding; Novartis: Consultancy; Jazz: Consultancy, Research Funding. Thepot:astellas: Honoraria; novartis: Honoraria; sanofi: Honoraria; celgene: Honoraria. Giagounidis:AMGEN: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees. Luebbert:Janssen: Research Funding. Park:Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Other: Travel expenses. Stamatoulas Bastard:Pfizer: Other: TRAVEL, ACCOMMODATIONS, EXPENSES; Celgene: Honoraria; Takeda: Consultancy. Solary:Janssen: Research Funding. Platzbecker:Novartis: Consultancy, Honoraria, Research Funding; BMS: Consultancy, Honoraria; Amgen: Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria; Geron: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria. Fenaux:Novartis: Honoraria, Research Funding; Abbvie: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Jazz: Honoraria, Research Funding.
Decitabine for CMML with WBC > 13 x109/L.
Author notes
Asterisk with author names denotes non-ASH members.